Research Updates
Research Updates
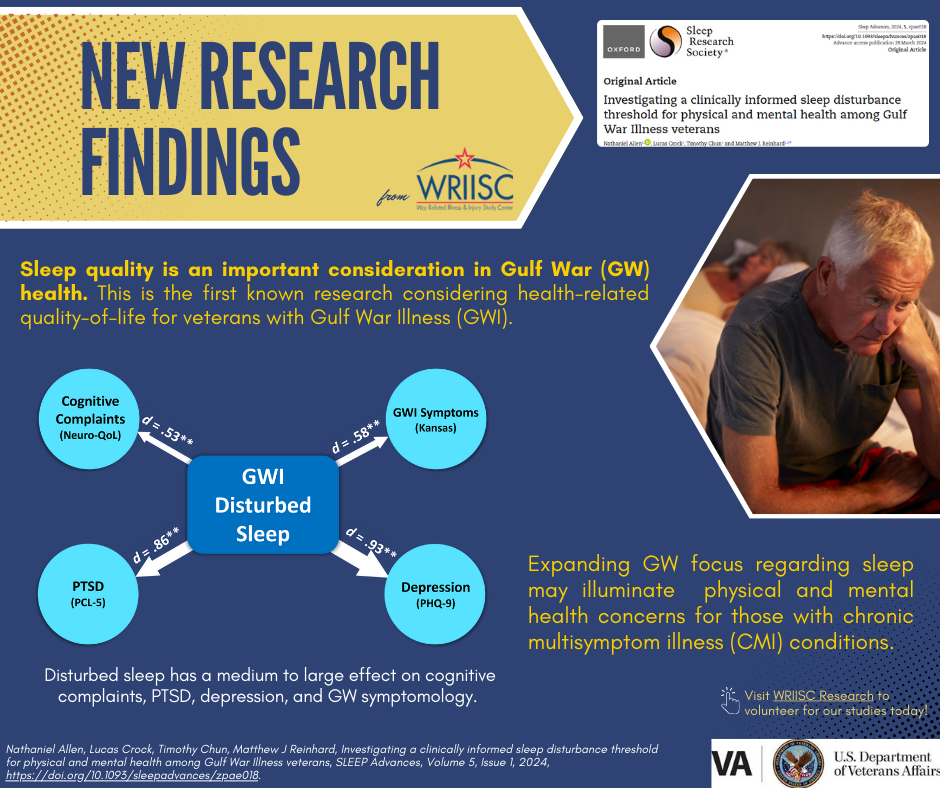
Click here for a graphical description of findings.
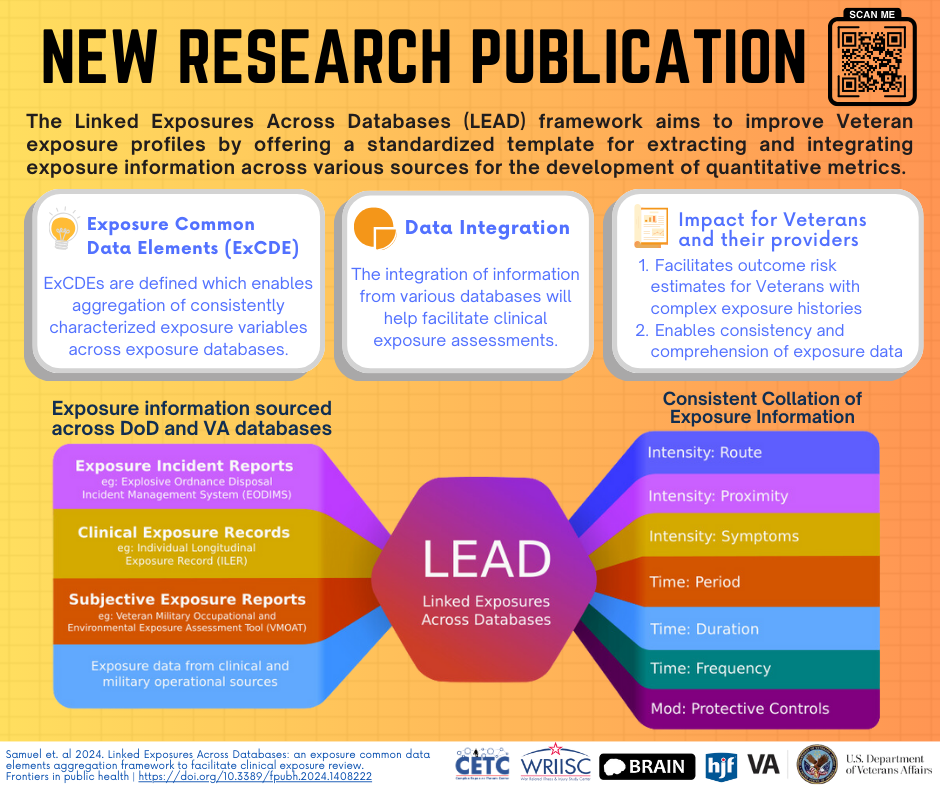
Click here to read.
Abstract Archives
- Symptom attribution to a medically unexplained syndrome is associated with greater perceived severity and bothersomeness of symptoms in US military veterans
- Understanding Veterans' Causal Attributions of Physical Symptoms
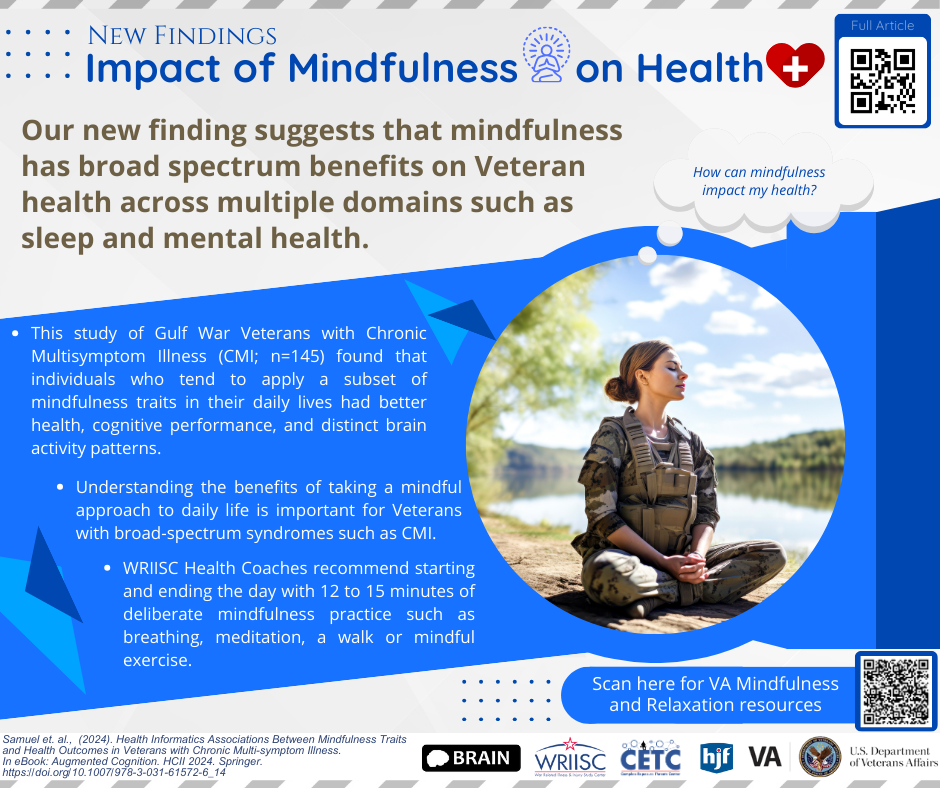
Click here for a graphical description of findings.
Click here to read. - Safety, Tolerability and Efficacy of Dietary Supplementation with Concord Grape Juice in Gulf War Veterans with Gulf War Illness
Click here for a graphical description of findings.
Click here to read. - Towards the objective assessment of suicidal states: Some neurocognitive deficits may be temporally related to suicide attempt
Click here for a graphical description of findings.
Click here to read. - Mental Health Conditions and Hospitalizations for Ambulatory Care Sensitive Conditions Among Veterans with Diabetes
Click here for a graphical description of findings.
Click here to read. - Exercise-Induced Bronchoconstriction in Iraq and Afghanistan Veterans with Deployment-Related Exposures
Click here for a graphical description of findings.
Click here to read. - Post-Exertional Malaise in Veterans with Gulf War Illness
Click here for a graphical description of findings.
Click here to read. - Doctor Recommendations are Related to Patient Interest and Use of Behavioral Treatment for Chronic Pain and Addiction
Click here for a graphical description of findings.
Click here to read. - Are Common Sense Model constructs and Self-Efficacy Simultaneously Correlated with Self-Management Behaviors and Health Outcomes: A Systematic Review
Click here for a graphical description of findings.
Click here to read. - Coping with Medically Unexplained Physical Symptoms: The Role of Illness Beliefs and Behaviors
Click here for a graphical description of findings.
Click here to read. - Progression of Intervention-Focused Research for Gulf War Illness
Click here for a graphical description of findings.
Click here to read. - Impact of presumed service-connected diagnosis on the Department of Veterans Affairs healthcare utilization patterns of Vietnam-Theater Veterans
Click here for a graphical description of findings.
Click here to read.